Parkinson’s disease (PD) is a progressive neurodegenerative disorder affecting movement, sleep, mood, and overall quality of life. Standard treatments like levodopa provide relief for motor symptoms, but many patients continue to struggle with non-motor issues such as anxiety, insomnia, and chronic pain. In recent years, cannabis and Parkinson’s disease has become a major research focus, with medical marijuana gaining attention as a potential therapy. Many patients wonder: does cannabis help Parkinson’s symptoms? With new studies published between 2023 and 2025 on PubMed, as well as findings from clinical trials and patient surveys, researchers now have a clearer picture of where cannabinoids such as CBD and THC may help Parkinson’s patients, where they may fall short, and what we can expect from future treatments.
Quick Answers:
- Does cannabis help Parkinson’s? Yes, for non-motor symptoms like sleep and anxiety
- Medical marijuana Parkinson’s: Legal in 47 states
- Parkinson’s tremor cannabis effectiveness: Limited and inconsistent
- CBD for Parkinson’s safety: Generally safer than THC
Understanding Cannabis and the Brain
The Endocannabinoid System
Before diving into the research, it helps to understand why cannabis affects the brain at all. The human body contains an endocannabinoid system (ECS), a complex network of receptors found throughout the nervous system. This system naturally regulates functions including mood, pain perception, memory, appetite, and sleep.
The ECS consists of:
- Cannabinoid receptors (CB1 and CB2) expressed throughout the brain and body
- Endocannabinoids – natural chemicals your body produces that bind to these receptors
- Enzymes that break down endocannabinoids after use
The chemicals in cannabis can mimic these naturally occurring compounds, binding to the same receptors and influencing the same systems. This is why cannabis can affect mood, pain, and other symptoms relevant to Parkinson’s disease.
CBD for Parkinson’s: Why It’s Safer Than THC
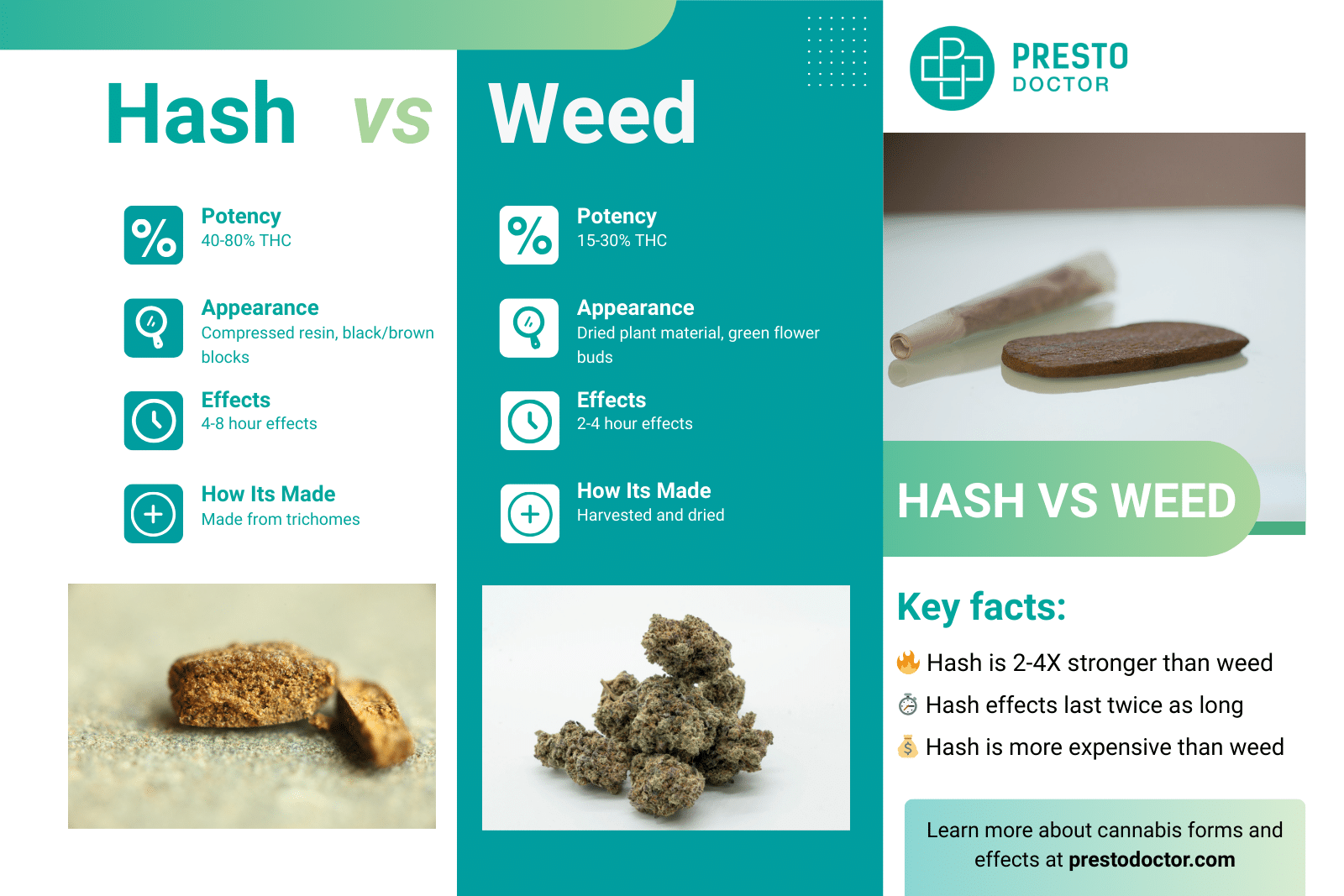
Cannabis contains over 60 active compounds called cannabinoids, but two have been most studied for their potential role in Parkinson’s disease:
THC (Δ⁹-tetrahydrocannabinol): The psychoactive compound that produces the “high” associated with marijuana. May help with pain, muscle stiffness, and sleep, but carries risks for cognition and mood, particularly in elderly patients.
CBD (cannabidiol): Non-psychoactive compound that does not produce intoxication. Shows promise for reducing anxiety, psychosis, and improving sleep without cognitive impairment.
THC:CBD combinations: Formulations containing both cannabinoids, with effects varying depending on the ratio. Many medical cannabis products use ratios such as 1:1, 1:20 (high CBD), or 20:1 (high THC).
Delivery Methods
Medical cannabis comes in several forms, each with different onset times and duration:
- Oils and tinctures: Taken under the tongue; effects begin in 15-45 minutes
- Capsules: Swallowed like pills; slower onset (1-2 hours) but longer duration
- Vaporizers: Inhaled vapor (not smoke); fastest onset (minutes) but shortest duration
- Nasal sprays: Absorbed through nasal membranes; moderate onset time
- Edibles: Not recommended for medical use due to unpredictable absorption
Most clinical studies use oils or capsules for consistent dosing.
How Cannabis and Parkinson’s Interact: Effects on Symptoms
Motor Symptoms (Tremor, Rigidity, Slowness)
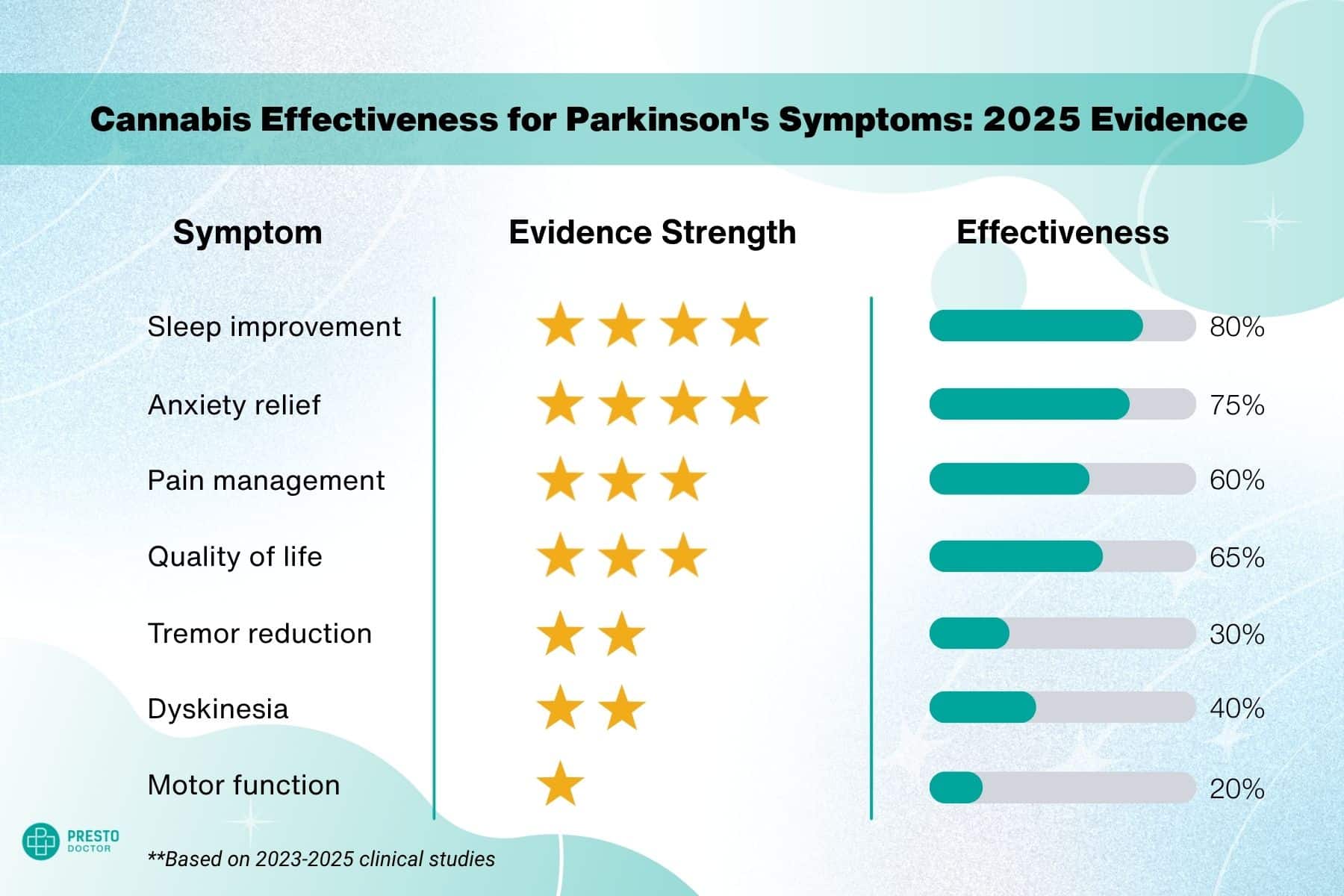
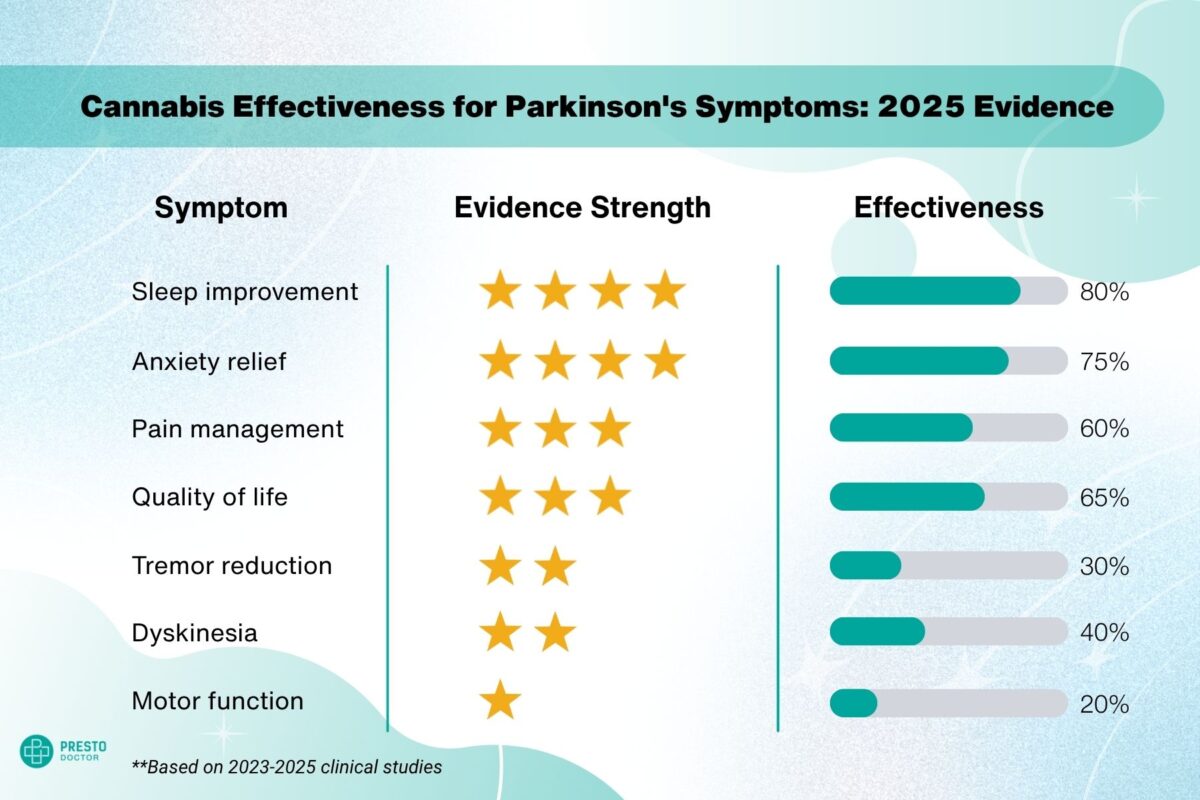
A 2023 retrospective chart review of 69 Parkinson’s patients using cannabis treatments reported improvements in tremor, spasticity, and dystonia. However, cannabis effectiveness in Parkinson’s tremors remains inconsistent in controlled trials.
However, randomized controlled trials have shown mixed results, with many reporting no significant improvement in motor function.
While cannabis and Parkinson’s motor symptoms show mixed results, non-motor benefits are more promising. Medical marijuana patients with Parkinson’s report significant sleep improvements.”
Takeaway: Cannabis may provide mild benefit for some motor symptoms, but it is not as reliable as standard PD medications. The Parkinson’s Foundation consensus statement emphasizes that cannabis should never be considered a replacement for dopaminergic therapies like levodopa.
Non-Motor Symptoms (Sleep, Pain, Anxiety, Cognition)
Sleep: A 2025 case series using THC+CBD extracts showed significant improvement in insomnia after approximately 60 days of treatment. Sleep disturbance is one of the most commonly reported benefits among PD patients using cannabis.
Anxiety & Mood: Studies with nabilone (a synthetic THC analog) and CBD report reductions in anxiety and better quality of life scores. Given that anxiety affects up to 40% of people with Parkinson’s, this represents a significant potential benefit.
Pain: Surveys from the Michael J. Fox Foundation (MJFF) highlight cannabis as a popular tool for pain management among PD patients. Chronic pain affects approximately 85% of people with Parkinson’s at some point.
Cognition: Evidence is mixed and concerning. Some studies suggest improvements, while others found worse MoCA (cognitive screening) scores, especially in patients using THC-heavy products. This is particularly important because Parkinson’s disease already affects executive function—the ability to plan, make decisions, and control impulses.
Takeaway: Cannabis appears most promising for non-motor symptoms, particularly sleep, anxiety, and pain relief. However, cognitive risks must be carefully weighed, especially in older adults.
Levodopa-Induced Dyskinesia
Some observational studies suggest cannabis may reduce levodopa-induced dyskinesias (involuntary movements caused by long-term levodopa use).
Evidence remains preliminary, and more placebo-controlled clinical trials are needed.
Key Findings from Recent Studies (2023–2025)
| Year | Study | Findings |
|---|---|---|
| 2025 | Ruver-Martins et al. | THC+CBD extract improved insomnia; trend toward better cognition |
| 2024 | Liu et al. (CBD+THC trial) | Well-tolerated; mixed effects on motor function |
| 2023 | Aladeen et al. | 69 PD patients—reported improvements in both motor & non-motor symptoms; reduced opioid use |
| 2023 | Sousa et al. | Users reported better sleep and anxiety relief, but worse cognitive scores |
Real-World Usage Data
According to surveys conducted by the Parkinson’s Foundation at 40 Centers of Excellence:
- 80% of people with Parkinson’s have tried cannabis at some point
- 95% of neurologists report being asked about cannabis by their patients
- Only 10-11% of neurologists have actually recommended cannabis to patients
- 23% of physicians have received any formal education on medical cannabis
- 93% of physicians want cannabis education included in medical training
This gap between patient interest and physician comfort highlights the need for more rigorous research in addition to medical education.
Safety and Side Effects
Most studies show cannabis and cannabinoids are well tolerated, but side effects do occur:
Common side effects:
- Drowsiness and fatigue
- Memory and concentration difficulties
- Dizziness or lightheadedness
- Dry mouth
More serious concerns:
- Mood changes (anxiety, paranoia—especially with THC-dominant products)
- Impaired balance and coordination
- Hallucinations (rare, but higher risk in elderly)
- Apathy or reduced motivation with long-term use
In clinical trials: 4 out of 69 patients in one study discontinued cannabis due to adverse effects—a relatively low rate compared to many medications.
Special Risks for Parkinson’s Patients
Executive function impairment: Parkinson’s disease can already impair executive function. Cannabis, particularly THC, can compound this effect. The combination may increase risky decision-making and poor judgment.
Elderly patients: People over 65 are more susceptible to cognitive side effects, confusion, and falls. Start with very low doses if considering cannabis.
Drug interactions: Cannabis can interact with:
- Blood thinners (warfarin, apixaban): May increase bleeding risk
- Sedatives and sleep medications: Additive drowsiness
- Antidepressants: Potential mood effects
- Other medications metabolized by liver enzymes
Always disclose cannabis use to all your healthcare providers.
QUESTION: Can I use cannabis if I’m taking blood thinners for Parkinson’s? Only under medical supervision. Cannabis may interact with blood thinners like warfarin, potentially increasing bleeding risk. Always discuss with your doctor before combining medications.
Current Clinical Trials to Watch
Several important studies are currently underway or recently completed:
CAN-PDP (United Kingdom): Testing cannabidiol (CBD) specifically for Parkinson’s disease psychosis, which affects up to 50% of patients in later stages.
NCT05106504: Evaluating cannabis for non-motor symptoms including insomnia and anxiety in people with Parkinson’s.
MJFF-sponsored observational studies: Collecting real-world patient data on cannabis use patterns, benefits, and side effects in PD.
These trials may provide more definitive answers on optimal dosing, which symptoms respond best, and which formulations are most effective.
Legal and Regulatory Status
United States
Federal status: Cannabis remains a Schedule I controlled substance under federal law, meaning it is considered to have no accepted medical use and high potential for abuse. This classification limits research funding and also makes large-scale clinical trials difficult.
State laws: As of 2025, medical cannabis is available in some form in 47 states:
- 24 states: Full legalization (both medical and recreational)
- 14 states: Medical cannabis legal only
- 9 states: Only CBD/low-THC products legal
- 3 states: No legal cannabis provisions
Prescription vs. recommendation: Because cannabis is federally illegal, physicians cannot write prescriptions. Instead, they provide written recommendations or certifications that allow patients to purchase from state-licensed dispensaries.
Parkinson’s disease is specifically listed as a qualifying condition in most states with medical cannabis programs.
International
Several countries allow medical cannabis for Parkinson’s disease, including Canada, Germany, and the United Kingdom, though regulations and availability vary.
QUESTION: Are cannabis-based drugs FDA approved for Parkinson’s disease? No. While some cannabinoid medications are FDA-approved for other conditions, none are specifically approved for Parkinson’s disease. This means no standardized dosing guidelines exist.
How Cannabis Compares to Standard Treatment
Levodopa: Remains the gold standard for motor symptoms. Cannabis does not replace levodopa or other dopaminergic medications.
Cannabis: Shows more promise for non-motor symptoms (sleep, anxiety, pain, quality of life) that standard medications don’t adequately address.
Best use case: Adjunctive (add-on) therapy for specific symptoms, not as a standalone treatment. Cannabis should be viewed as one tool in a comprehensive treatment plan.
Dosage Guidelines from Clinical Studies
While optimal dosing remains unclear, clinical trials have used these ranges:
CBD:
- Starting dose: 5-10 mg daily
- Therapeutic range in studies: 75-300 mg daily
- Maximum studied: 600 mg daily
THC:
- Starting dose: 1-2.5 mg daily (particularly important for elderly)
- Therapeutic range: 2.5-20 mg daily
- Higher doses increase psychoactive effects and side effects
CBD:THC combinations:
- Many studies use 1:1 ratios
- Higher CBD ratios (e.g., 20:1) reduce psychoactive effects
Note that these are research ranges only – work with a physician familiar with medical cannabis to determine appropriate dosing for your specific situation.
When determining CBD or medical marijuana dosage for Parkinson’s treatment plans, start conservatively.
QUESTION: How much CBD oil should I take for Parkinson’s tremors? Start with 5-10mg of CBD daily and increase by 5-10mg every week while monitoring effects. Clinical studies for Parkinson’s symptoms use 75-300mg daily, though tremor response is inconsistent. Work with your neurologist to find the right dose, as CBD doesn’t reliably reduce tremors in most patients.
Cannabis and Parkinson’s: Practical Tips for Patients
Before starting anything new such as medical marijuana treatment for Parkinson’s, consult with your physician or a movement disorder specialist to consider the CBD vs THC options.
Before Starting
- Consult your neurologist first. Discuss whether your specific symptoms might benefit and review your full medication list for interactions.
- Check your state’s laws. Determine if you need a formal certification and how to access legal dispensaries.
- Consider your risk factors. Cannabis may not be appropriate if you have:
- History of psychiatric illness (schizophrenia, psychosis)
- Significant cognitive impairment
- History of substance abuse
- Cardiovascular disease
Starting Cannabis
- Start low, go slow. Begin with the lowest available dose, particularly for THC. Wait at least a week before increasing.
- Prefer higher CBD ratios. CBD-dominant products (20:1 or higher) minimize psychoactive risks while still providing potential benefits.
- Use regulated, tested products. Purchase only from licensed dispensaries with lab-tested products showing exact cannabinoid content and screening for contaminants.
- Choose consistent delivery methods. Oils and capsules provide more predictable effects than smoking or edibles.
Monitoring Your Response
- Track your symptoms systematically. Use a diary or app to record:
- Dose and timing
- Symptom changes (positive and negative)
- Side effects
- Changes in other medications
- Watch for cognitive changes. Have family members help monitor for confusion, poor judgment, or personality changes.
- Report back to your physician regularly. Treat cannabis like any other medication—assess benefits and also risks at follow-up appointments.
- Be patient. Some benefits (particularly for sleep and anxiety) may take 4-8 weeks to fully manifest.
- Don’t stop other medications. Continue your standard Parkinson’s medications unless specifically instructed otherwise by your neurologist.
What Major Parkinson’s Organizations Say
Parkinson’s Foundation Position: The Foundation’s consensus statement from 46 experts emphasizes that cannabis should never replace standard dopaminergic therapies. They call for more research, particularly large-scale clinical trials with rigorous methodology. They note the lack of dosage guidelines and timing instructions makes physician recommendations difficult.
American Parkinson Disease Association (APDA): APDA takes a measured approach, noting that while some data suggests benefits for quality of life, dyskinesia, pain, anxiety, and sleep, more robust clinical trials are needed. They emphasize treating cannabinoids like any other medication requiring evidence-based evaluation.
Michael J. Fox Foundation: MJFF actively funds research into cannabis for Parkinson’s, including large observational studies tracking real-world use patterns. They maintain that well-designed clinical trials are essential before cannabis can be recommended as standard care.
All three major organizations emphasize that medical marijuana for Parkinson’s treatment requires more research. When asked ‘does cannabis help Parkinson’s?’ they cite limited evidence for motor symptoms. The consensus: CBD for Parkinson’s may help non-motor symptoms, but cannabis helping with Parkinson’s tremors lack robust support.
Frequently Asked Questions: Cannabis and Parkinson’s Disease
Cannabis does not reliably help Parkinson’s tremors. While some patients report improvement, clinical trials have not confirmed consistent benefits for tremor reduction. Traditional medications like levodopa remain more effective for motor symptoms.
Yes, CBD is generally safer for Parkinson’s patients. It has fewer cognitive side effects and no psychoactive effects, while THC poses more risks for confusion, mood changes, and balance problems in elderly patients.
Possibly. Some studies suggest cannabis may reduce dyskinesia from levodopa, but evidence is preliminary. More randomized controlled trials are needed to confirm this benefit.
Cannabis shows most promise for non-motor symptoms: sleep disturbances, anxiety, chronic pain, and quality of life. Evidence for motor symptoms like tremor is inconsistent.
Higher CBD ratios (20:1 or pure CBD) are recommended to minimize side effects. Use 1:1 ratios only for pain or sleep at night. Start with high CBD ratios and adjust under medical supervision.
No. Cannabis cannot replace levodopa, which remains the gold standard for motor symptoms. Cannabis is best used as an add-on therapy for symptoms like sleep, anxiety, or pain.
Yes, cannabis shows promise for pain management. Studies show reduced opioid use among cannabis users, and surveys indicate it’s popular for pain relief, though more research is needed for optimal dosing.
Yes, marijuana shows significant promise for Parkinson’s sleep issues. A 2025 study found THC+CBD extracts improved insomnia after 60 days of treatment. Sleep disturbance is one of the most commonly reported benefits among Parkinson’s patients using cannabis.
Medical Marijuana for Parkinson’s
Medical marijuana is not a cure for Parkinson’s disease, but evidence increasingly supports its potential role in managing non-motor symptoms such as insomnia, anxiety, pain, and quality of life issues.
Motor symptom improvements remain inconsistent, and potential cognitive side effects are a legitimate concern—particularly with THC-heavy products in elderly patients.
With larger clinical trials now underway, the coming years should provide more definitive answers about the role of THC, CBD, and cannabis extracts in Parkinson’s care. As support for medical marijuana grows in more states, Parkinson’s patients may have more options to experiment with CBD and THC for relief.
Current bottom line: Cannabis should be considered a potentially useful add-on therapy for specific symptoms, ideally used under the guidance of a movement-disorder specialist who can monitor both benefits and risks. It is not a replacement for proven treatments like levodopa, but for patients struggling with pain, sleep, or anxiety despite standard care, medical cannabis may offer meaningful relief. While evidence for cannabis helping with Parkinson’s tremors, CBD may help with Parkinson’s related sleep problems and anxiety.
As with any medical decision, the choice to try cannabis should be individualized, based on your specific symptoms, risk factors, and also response to treatment—made in partnership with your healthcare team.
| Question | Answer |
|---|---|
| Does cannabis help Parkinson’s tremors? | Parkinson’s tremor cannabis research shows inconsistent results |
| Is CBD for Parkinson’s safe? | CBD for Parkinson’s is generally safer than THC |
| Does medical marijuana help? | Medical marijuana Parkinson’s patients report benefits for sleep and pain |
| What works best? | CBD for Parkinson’s anxiety and sleep shows most promise |
Additional Resources
- Parkinson’s Foundation Consensus Statement on Medical Cannabis: Download PDF
- APDA Cannabis and Parkinson’s Guide: Visit APDA
- State-by-State Legal Guide: NORML.org/laws
- Michael J. Fox Foundation Research Updates: Search clinical trials
- Clinical Trials Database: ClinicalTrials.gov – Search “cannabis Parkinson’s”
This article is for informational purposes only and does not constitute medical advice. Always consult with your neurologist or movement disorder specialist before starting any new treatment, including medical cannabis.