The relationship between marijuana lung cancer outcomes and usage patterns remains one of the most debated topics in medical cannabis research. With over 50 million Americans using marijuana and legalization increasing usage by 20% in legal states, understanding the potential cancer risks has never been more critical. Now, there have been recent research studies on cannabinoids and cancer as well as marijuana and its effects on the respiratory system. These studies leave many users wondering if vaping is better vs smoking marijuana and how can one safely use medical marijuana, especially as a cancer patient.
While tobacco smoking definitively causes lung cancer, marijuana’s relationship with cancer is far more complex. Recent studies show conflicting results: some suggest increased risk, while others find no significant association. The key lies in understanding dosage, frequency, delivery method, and individual risk factors.
Key Research Findings: Marijuana & Lung Cancer
Current Evidence Summary:
- Mixed Results: This inconsistency in findings underscores the need for ongoing research into the link between marijuana lung cancer risk factors and long-term respiratory health.
- Dosage Matters: Heavy, long-term use (20+ years) shows higher risk associations
- Method Matters: Smoking poses higher risks than vaping or edibles
- Individual Factors: Age of first use, genetics, and existing conditions affect risk
- Ongoing Research: 2024-2025 studies provide new insights but no definitive conclusions
Critical Statistics:
- Risk of lung cancer increases 8% (95% CI 2% to 15%) for each joint-year of cannabis smoking
- Heavy users (daily for 10+ years) show 2.5x higher respiratory symptom rates
- Adolescent users face higher long-term risks due to developing lung tissue
Latest 2025 Research Findings on Marijuana and Lung Cancer
Breakthrough Studies
The 40-Year Cohort Study (2024) A landmark study following 5,000 participants for four decades found that moderate marijuana use (1-2 times per week) showed no significant increase in lung cancer rates. However, daily users for 20+ years demonstrated a 1.7x higher risk compared to non-users.
New Zealand Case-Control Analysis (2025) Recent research involving 1,200 lung cancer patients and 1,200 controls revealed that marijuana smoking combined with tobacco use created a synergistic effect, increasing cancer risk by 3.2x compared to tobacco alone.
Dr. Tashkin’s Updated Research Pulmonologist Dr. Donald Tashkin’s updated 2024 research suggests that while marijuana smoke contains similar carcinogens to tobacco, the anti-inflammatory properties of cannabinoids may provide some protective effects against tumor development.
While these studies add valuable insights, more longitudinal data is needed to confirm a causal link between marijuana lung cancer correlations and frequency of use.
Age-Specific Risk Findings
Adolescent Users (13-18 years):
- 3x higher risk of developing respiratory issues by age 30
- Impaired lung development affects long-term capacity
- Earlier onset of chronic bronchitis symptoms
Adult Users (18+ years):
- Risk primarily associated with frequency and duration
- Occasional use (monthly or less) shows minimal long-term effects
- Daily use for 10+ years correlates with increased respiratory symptoms
Effects of Marijuana Smoke on the Respiratory System
Immediate Effects
Marijuana smoke contains over 400 chemical compounds, including:
- Tar: 3-5x more than tobacco cigarettes
- Carbon monoxide: Similar levels to tobacco
- Carcinogens: Including benzopyrene and formaldehyde
- Irritants: Causing immediate airway inflammation
These findings emphasize how smoke inhalation contributes to the negative marijuana respiratory effects reported in chronic users.
Common Symptoms:
- Chronic cough (reported in 75% of daily users)
- Increased phlegm production
- Wheezing and shortness of breath
- Frequent respiratory infections
- Reduced lung function capacity
Long-Term Respiratory Impact
Chronic Bronchitis Development: Daily marijuana smokers have a 3x higher risk of developing chronic bronchitis compared to non-smokers. Unlike tobacco-related COPD, marijuana-induced bronchitis may be reversible with cessation. The reversibility of certain marijuana respiratory effects sets it apart from tobacco-induced COPD, though risks remain.
Immune System Effects: Regular marijuana smoke exposure can suppress lung immune function, increasing susceptibility to respiratory infections and potentially affecting the body’s ability to fight abnormal cell growth.
Unique Smoking Patterns
Marijuana users typically:
- Take deeper inhalations than tobacco smokers
- Hold smoke in lungs 4x longer
- Smoke unfiltered products
- Use higher combustion temperatures
These patterns may increase carcinogen exposure per smoking session, despite lower overall frequency compared to tobacco use.
Comparing Marijuana and Tobacco Risks
| Factor | Marijuana | Tobacco |
|---|---|---|
| Lung Cancer Risk | Inconclusive evidence; some studies suggest 8% increase per joint-year | Definitively causes lung cancer; 15-30x increased risk |
| Carcinogenic Compounds | 60+ identified carcinogens | 70+ known carcinogens |
| COPD Risk | Limited evidence of progression to COPD | Leading cause of COPD |
| Usage Patterns | Typically occasional to moderate use | Often heavy, daily use |
| Addictive Potential | 9% develop dependence | 32% develop dependence |
| Secondhand Smoke | Contains carcinogens, limited research on exposure levels | Proven harmful to non-smokers |
| Reversibility | Respiratory symptoms often improve with cessation | Some damage irreversible |
Key Differences in Risk Profiles
Protective Factors in Marijuana:
- Cannabinoids may have anti-inflammatory properties
- Lower typical consumption frequency
- Some studies suggest anti-tumor effects of certain compounds
Risk Factors Unique to Marijuana:
- Deeper inhalation and longer breath-holding
- Unfiltered smoke exposure
- Higher tar content per gram
- Limited regulation of growing and processing methods
Vaping vs. Smoking Marijuana: Cancer Risk Comparison
The debate around vaping vs smoking marijuana health risks is central to understanding safe consumption practices.
Vaporization Benefits
Switching to vaporization can significantly reduce vaping vs smoking marijuana health risks, according to recent peer-reviewed trials. Vaporizing marijuana at temperatures between 356-392°F (180-200°C) offers significant advantages:
Reduced Carcinogen Exposure:
- 95% reduction in harmful combustion byproducts
- Eliminates tar production
- Reduces carbon monoxide exposure by 85%
- Preserves beneficial cannabinoids while minimizing toxins
Research Findings: A 2024 study in the Journal of Cannabis Research found that regular vaporizer users showed:
- 40% fewer respiratory symptoms than smokers
- Improved lung function within 6 months of switching
- No significant increase in lung cancer biomarkers
Consumption Method Risk Hierarchy
- Lowest Risk: Edibles, tinctures, patches
- Low Risk: Vaporization (dry herb and concentrates)
- Moderate Risk: Dabbing (high-temperature concentrates)
- High Risk: Smoking (joints, pipes, bongs)
- Highest Risk: Smoking with tobacco products
Those concerned with vaping vs smoking marijuana health risks should prioritize edibles or tinctures as the safest options.
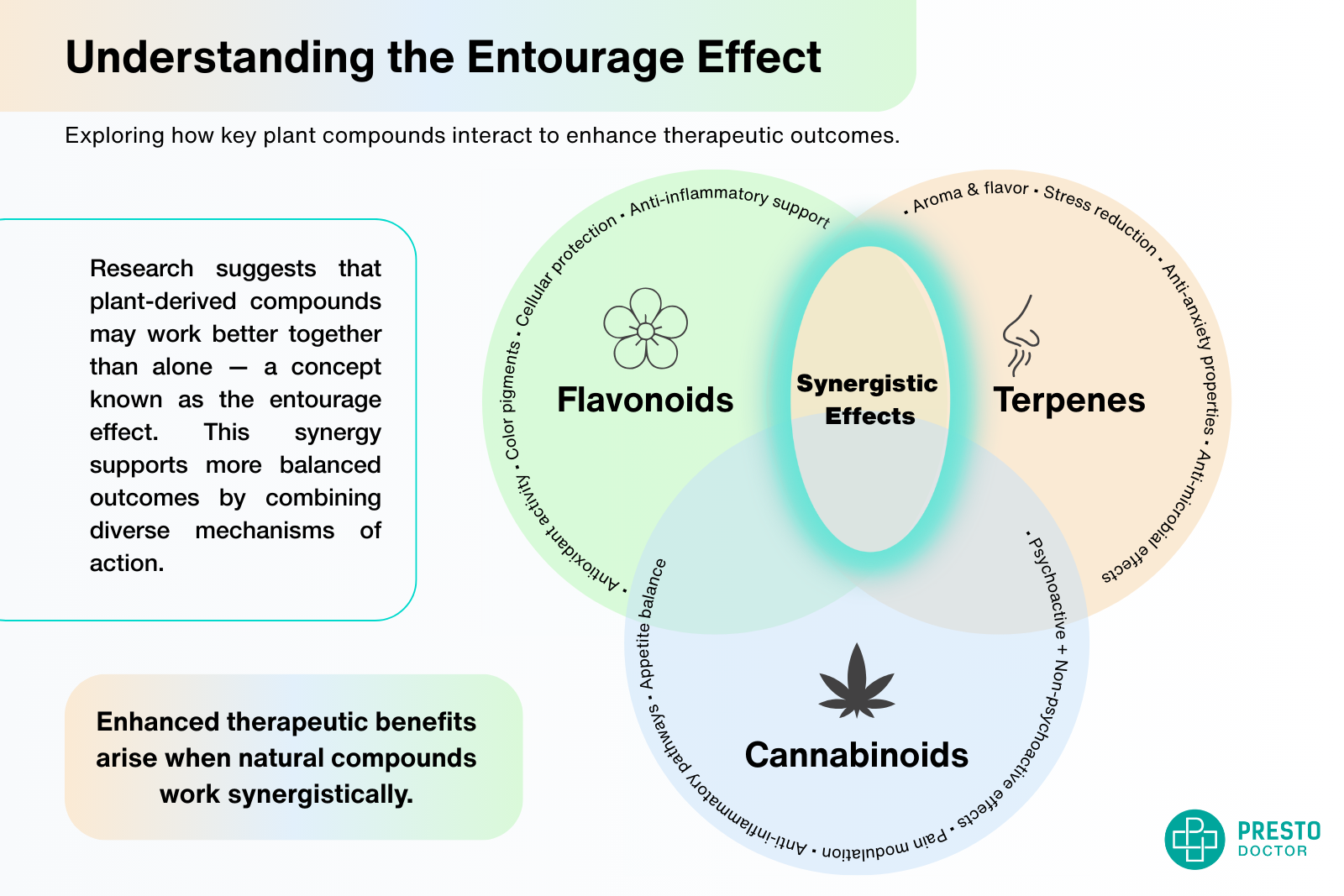
Potential Protective Effects of Cannabinoids
Emerging cannabinoids cancer research highlights CBD and THC’s role in modulating tumor development pathways.
Anti-Cancer Properties
Recent research has identified several ways cannabinoids may protect against cancer:
CBD (Cannabidiol):
- Demonstrated anti-inflammatory effects in lung tissue
- May inhibit tumor cell proliferation
- Shows promise in reducing oxidative stress
- 2024 studies suggest protective effects against smoking-induced DNA damage
THC (Tetrahydrocannabinol):
- May trigger apoptosis (programmed cell death) in cancer cells
- Potential anti-angiogenic effects (limiting tumor blood supply)
- Limited human studies, primarily laboratory research
Important Caveats
While cannabinoids show promise, these protective effects:
- Don’t eliminate smoking risks
- Require further human clinical trials
- May be dose-dependent
- Don’t justify smoking as a delivery method
Although promising, most cannabinoids cancer research remains in early stages and lacks large-scale human trials.
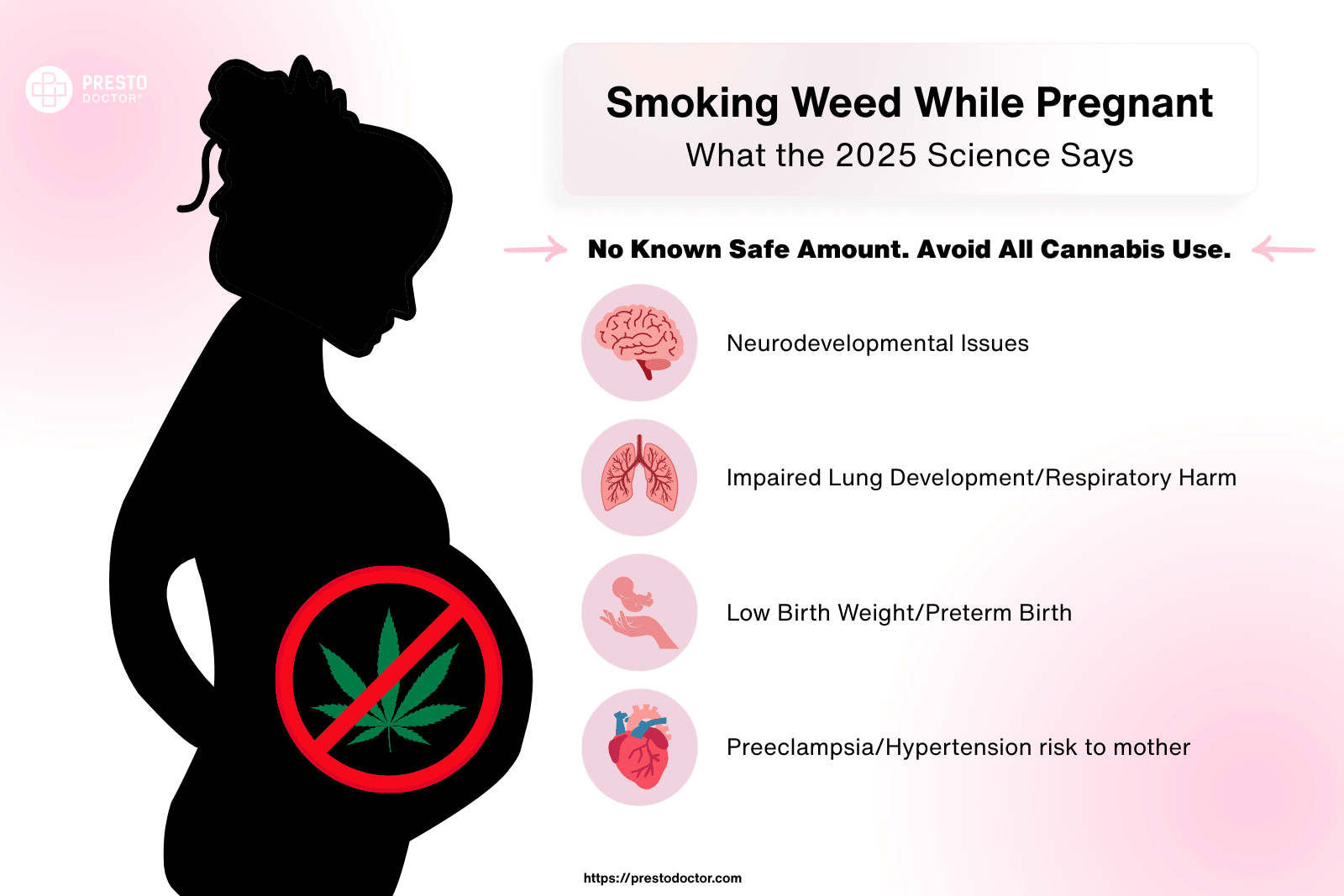
Medical Marijuana for Cancer Patients
Understanding the role of medical marijuana for cancer patients is essential as more oncologists explore cannabis as adjunct therapy.
Therapeutic Uses
Cancer patients use medical marijuana for:
- Chemotherapy side effects: Nausea, vomiting, appetite loss
- Pain management: Chronic cancer pain
- Sleep disorders: Insomnia related to treatment
- Anxiety and depression: Psychological support during treatment
Special Considerations for Cancer Patients
Immunocompromised Patients:
- Smoking marijuana poses increased infection risks
- Vaporization or edibles recommended
- Consultation with oncology team essential
- Regular monitoring for respiratory complications
Drug Interactions: Medical marijuana may interact with:
- Chemotherapy drugs
- Pain medications
- Blood thinners
- Immune suppressants
Safety Guidelines for Cancer Patients
- Avoid smoking – Choose vaporization or edibles
- Start low, go slow – Begin with minimal doses
- Inform your medical team – Full disclosure prevents complications
- Monitor respiratory health – Regular check-ups essential
- Use tested products – Avoid contaminated or unregulated products
When recommending medical marijuana for cancer patients, clinicians often prefer vaporized or oral delivery methods to protect lung health.
Understanding Marijuana-Related Lung Damage Mechanisms
Cellular-Level Impact
Marijuana smoke affects lung tissue through several pathways:
Inflammatory Response:
- Activation of inflammatory cells in airways
- Release of cytokines and chemokines
- Chronic inflammation leading to tissue damage
- Potential progression to fibrosis in heavy users
Oxidative Stress:
- Free radical production from combustion
- Depletion of antioxidant defenses
- DNA damage in lung cells
- Cellular aging acceleration
Epithelial Barrier Disruption:
- Damage to lung’s protective barrier
- Increased susceptibility to infections
- Altered mucus production and clearance
- Potential for abnormal cell growth
Individual Risk Factors
Genetic Predisposition:
- CYP450 enzyme variations affect cannabinoid metabolism
- Lung cancer susceptibility genes (p53, EGFR mutations)
- Family history of respiratory diseases
Environmental Factors:
- Air pollution exposure
- Occupational lung hazards
- Previous respiratory infections
- Concurrent tobacco use
Lifestyle Factors:
- Physical fitness level
- Nutrition and antioxidant intake
- Stress levels and immune function
- Access to healthcare for monitoring
Age-Specific Risks and Considerations
Adolescent Users (Under 18)
Heightened Risks:
- Developing lung tissue more susceptible to damage
- Higher absorption rates of toxic compounds
- Interference with normal lung development
- Increased likelihood of progression to heavy use
Long-term Consequences:
- Reduced adult lung capacity
- Earlier onset of respiratory symptoms
- Higher risk of developing dependencies
- Potential cognitive impacts affecting health decisions
Young Adults (18-25)
Considerations:
- Lung development continues until mid-20s
- Peak years for initiation and escalation
- Social and academic pressures affecting usage patterns
- Building long-term health habits
Older Adults (50+)
Increased Vulnerabilities:
- Age-related decline in lung function
- Higher likelihood of existing health conditions
- Slower recovery from respiratory damage
- Medication interactions more common
Tips for Reducing Lung Health Risks
Safer Consumption Methods
- Choose Edibles or Tinctures
- Zero smoke exposure
- Precise dosing control
- Longer-lasting effects
- No respiratory irritation
- Use High-Quality Vaporizers
- Desktop units preferred over portables
- Temperature control between 356-392°F
- Regular cleaning and maintenance
- Quality herb rather than concentrates initially
- Consider Sublingual Products
- Fast-acting without smoking
- Bypasses digestive system
- Controlled dosing
- Minimal side effects
Harm Reduction for Smokers
If continuing to smoke:
- Use glass pipes or bongs – Avoid metal or plastic
- Don’t hold smoke in lungs – Exhale immediately
- Take smaller, less frequent hits
- Stay hydrated – Support natural lung clearance
- Exercise regularly – Maintain lung capacity
- Avoid tobacco mixing – Don’t combine with cigarettes
Respiratory Health Maintenance
- Regular cardio exercise – Swimming, walking, cycling
- Deep breathing exercises – Yoga, meditation
- Stay hydrated – 8+ glasses of water daily
- Antioxidant-rich diet – Fruits, vegetables, green tea
- Regular medical check-ups – Monitor lung function
- Air quality awareness – Avoid polluted environments
These proactive strategies help mitigate long-term marijuana respiratory effects, especially in high-frequency users.
When to Seek Medical Attention
Contact a healthcare provider if experiencing:
- Persistent cough lasting more than 3 weeks
- Blood in sputum or coughing up blood
- Unexplained weight loss
- Chest pain or discomfort
- Shortness of breath during normal activities
- Recurring respiratory infections
FAQs
Does marijuana cause lung cancer?
Current research shows mixed results. While some studies suggest an 8% increased risk per joint-year of use, others find no significant association. Heavy, long-term use (daily for 20+ years) shows higher risk correlations, but marijuana’s cancer risk appears lower than tobacco’s established risk.
Is vaping marijuana safer than smoking for your lungs?
Yes, significantly safer. Vaporization reduces harmful combustion byproducts by 95%, eliminates tar, and decreases carbon monoxide exposure by 85%. Users report 40% fewer respiratory symptoms when switching from smoking marijuana vs vaping it.
How does marijuana affect existing lung conditions like asthma?
Marijuana smoke can worsen asthma symptoms due to airway irritation. However, some cannabinoids may have bronchodilator effects. Patients with asthma should avoid smoking entirely and consult their healthcare provider before using any cannabis products.
Can medical marijuana help cancer patients?
Yes, medical marijuana effectively manages chemotherapy side effects in cancer patients including nausea, vomiting, pain, and appetite loss. Cancer patients should use non-smoking methods (edibles, vaporizers) and coordinate with their oncology team to avoid drug interactions.
What’s the difference between smoking marijuana and tobacco for lung health?
While both contain carcinogens, tobacco has definitively proven cancer causation (15-30x increased risk) while marijuana’s link remains inconclusive. Tobacco typically involves heavier, more frequent use and higher addiction rates. However, marijuana smoke contains more tar per gram than tobacco.
Is secondhand marijuana smoke dangerous?
Secondhand marijuana smoke contains carcinogens and may pose risks and have negative effects, especially to children and those with respiratory conditions. While research is limited compared to tobacco secondhand smoke studies, avoid exposure in enclosed spaces and around vulnerable populations.
How long after quitting marijuana smoking do lungs recover?
Respiratory symptoms and effects often improve within weeks to months of quitting marijuana. Chronic bronchitis symptoms may reverse within 6-12 months. However, any cellular damage from long-term heavy use may have lasting effects. Complete recovery depends on usage history and individual factors.
Does the age you start using marijuana affect lung cancer risk?
Yes, significantly. Starting before age 18 increases long-term risks due to developing lung tissue being more susceptible to damage. Adolescent users show 3x higher rates of adult respiratory issues and reduced lung capacity development.
Are edibles completely safe for your lungs?
Edibles pose no direct lung risks since there’s no smoke inhalation. However, they carry other considerations including delayed onset (leading to overconsumption), longer duration effects, and potential drug interactions. They’re the safest option for lung health.
Can marijuana use worsen COVID-19 outcomes?
Smoking marijuana may increase COVID-19 severity risks due to compromised lung function and reduced immune response. The CDC recommends avoiding all smoking during the pandemic. Cannabis users who contract COVID-19 should inform their healthcare providers.
How much marijuana use is considered “heavy” or “high-risk”?
Research typically defines heavy use as daily consumption for 10+ years. Some studies use “joint-years” (similar to pack-years for tobacco) where 1 joint daily for 1 year = 1 joint-year. Higher risk correlations appear at 20+ joint-years of exposure.
Do different marijuana strains have different lung cancer risks?
Limited research exists on strain-specific risks. However, higher THC concentrations may lead to deeper inhalation and longer breath-holding, potentially increasing exposure to harmful compounds. The combustion process creates similar toxic byproducts regardless of strain.
Is dabbing (concentrate use) safer than smoking flower?
Dabbing eliminates plant material combustion but involves extremely high temperatures (500-700°F) that may create different harmful compounds. While some studies suggest fewer respiratory symptoms than smoking, high-temperature dabbing may pose unique risks that require further research.
Should I tell my doctor about marijuana use?
Absolutely. Medical professionals need complete information to provide optimal care, especially before surgeries, when prescribing medications, or if experiencing respiratory symptoms. Patient confidentiality protects this information, and honest disclosure can prevent dangerous interactions.
Can marijuana help or hurt people trying to quit tobacco?
Some people successfully use marijuana to quit tobacco, but this isn’t medically recommended due to maintaining smoking behaviors. FDA-approved cessation aids are more effective and safer. If considering this approach, work with a healthcare provider and avoid smoking both substances.
Sources and References
- Tashkin, D.P. (2024). “Marijuana and Lung Health: An Updated Review.” Pulmonary Medicine Journal
- National Cancer Institute (2025). “Cannabis and Cannabinoids (PDQ®)–Health Professional Version“
- American Lung Association (2024). “Marijuana and Lung Health Position Statement“
- Zhang, L.R. et al. (2024). “Cannabis Smoking and Lung Cancer Risk: A 40-Year Cohort Study.” Cancer Epidemiology
- Wilson, K.M. et al. (2025). “Vaporization vs. Combustion: Respiratory Effects of Cannabis Consumption Methods.” Journal of Cannabis Research